27 April 2021
Gainesville, FL, USA – A new University of Florida study of non-Hispanic Black and non-Hispanic white adults links, published in the Journal of Alzheimer's Disease, chronic knee pain and key demographic factors to differences in areas of the brain tied to memory. Participants who reported higher stages of pain and lower levels of income and education and less access to health insurance had thinner gray matter in these regions than those also experiencing higher stages of pain but who reported higher levels of income, education and greater access to health insurance.
Pain is a form of stress, both the symptoms and its effect on daily life. The research team has been investigating a new stage approach to measuring pain that characterizes chronic pain as a stressor based on factors that drive physiological change. These include frequency of pain (intermittent or persistent), average intensity of pain, duration of pain (how long living with pain), and extent of pain (number of pain sites across the body).
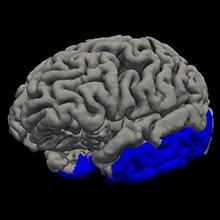
Participants with higher stages of pain and lower sociodemographic factors had about 4% less gray matter in the temporal lobe than participants in the same sociodemographic group with lower stages of pain.
“As we get older, typically starting around our mid-50s to mid-60s, we lose about half a percent of our gray matter per year,” said the study’s lead author Jared Tanner, PhD, a research assistant professor of clinical and health psychology in the UF College of Public Health and Health Professions, part of UF Health, the university’s academic health center. “So a 3–4% difference could be thought of as an additional six to eight years of aging in the brain.”
The area of the brain where the gray matter loss occurred is predictive of future cognitive decline, indicating these adults might have greater risk of developing dementia or Alzheimer’s disease, Tanner said.
“Other researchers have shown that non-Hispanic Black adults are up to twice as likely as non-Hispanic white adults to develop Alzheimer’s disease,” Tanner said. “Findings indicate a variety of environmental factors might be contributing. This study helps us begin to identify an additional factor to explore that may contribute to health disparities in rates of dementia and Alzheimer’s disease in some underrepresented ethnic/race groups. In this case, it looks like stage of chronic pain, along with other life experiences, may be playing a role.”
The study included 147 adults between the ages of 45 and 85 who experience mild to moderate knee pain. Participants were asked to provide sociodemographic information, complete a brief assessment of cognitive function and answer questions about their experience of knee pain intensity, frequency, how long it has been occurring and if they experience pain in other areas of their body. MRI scans captured images of their brains.
“The body and the brain are adaptive to stress to a certain point,” said the study’s senior author Kimberly Sibille, PhD, an associate professor of aging & geriatric research and pain medicine in the UF College of Medicine. “But with persistent stressors that are more intense and longer duration, eventually the body’s response is no longer adaptive and changes start occurring in the other direction, a process known as allostatic overload.
“We have previously shown relationships with stress-related clinical measures and now we show relationships in the brain,” Sibille said. “People with low pain stage – intermittent, low intensity, shorter duration and minimal sites of pain – differ from the groups with higher stages of chronic pain. Further, in combination with lower protective factors, including lower income, education and health insurance access, those individuals with higher chronic pain stage show less gray matter in cortical areas of the brain.”
While more research is needed to understand the complex relationship between the brain, pain and stress, the findings suggest that some individuals with chronic pain who are at increased risk for gray matter loss might benefit from earlier identification and treatment for their pain, Tanner said.
“I think what this research offers is further understanding of the consequences of chronic pain and associated risk and protective factors and approaches to improve how we assess chronic pain, which will hopefully inform our efforts to treat pain,” Sibille said.
Image credit: Jared Tanner, PhD
###
NOTES FOR EDITORS
Full study: "Relationships Between Chronic Pain Stage, Cognition, Temporal Lobe Cortex, and Sociodemographic Variables" by Jared J. Tanner, Shivani Hanchate, Catherine C. Price, Cynthia Garvan, Song Lai, Roland Staud, Hrishikesh Deshpande, Georg Deutsch, Burel R. Goodin, Roger B. Fillingim, and Kimberly T. Sibille (DOI: 10.3233/JAD-201345), published in the Journal of Alzheimer's Disease, Volume 80, Issue 4 (April 2021). The article is available online at: content.iospress.com/articles/journal-of-alzheimers-disease/jad201345.
Financial support for the study was provided by the National Institute on Aging and the Center for Advancing Translational Sciences, both part of the National Institutes of Health, as well as the National Science Foundation.
Contact
Further information can be obtained from media contact Ken Garcia (kdgarcia@ufl.edu or +1 3522659408). The press release was authored by Jill Pease, Public Relations Director, College of Public Health and Health Professions, University of Florida.
About the Journal of Alzheimer's Disease
Now in its 24th year of publication, the Journal of Alzheimer's Disease (JAD) is an international multidisciplinary journal to facilitate progress in understanding the etiology, pathogenesis, epidemiology, genetics, behavior, treatment, and psychology of Alzheimer's disease. The journal publishes research reports, reviews, short communications, book reviews, and letters-to-the-editor. Groundbreaking research that has appeared in the journal includes novel therapeutic targets, mechanisms of disease, and clinical trial outcomes. JAD has a Journal Impact Factor of 3.909 according to Journal Citation Reports (Clarivate, 2020). JAD is published by IOS Press. j-alz.com







