12 June 2020
Baseline MRIs Encouraged for COVID-19 Patients
Washington, DC, USA – The Journal of Alzheimer’s Disease has published a paper with a comprehensive review of the COVID-19’s effect on the nervous system which classifies brain damage caused by COVID-19 into three stages. One of the authors, nationally-recognized neurologist Dr. Majid Fotuhi, MD, PhD, who is the medical director of NeuroGrow Brain Fitness Center in Northern Virginia and an affiliate staff at Johns Hopkins Medicine, encourages the adoption of this three-stage classification, calls for more research on COVID-19's long-term effects on the brain, and stresses the need for patients to receive a brain MRI before leaving the hospital.
“We are learning that a significant number of hospitalized COVID-19 patients have various degrees of brain impairment. As a medical community, we need to monitor these patients over time as some of them may develop cognitive decline, attention deficit, brain fog, or Alzheimer’s disease in the future. There is a lot we can do to promote brain healing in COVID-19 patients, but first we must understand the nature and severity of their neurological deficits. At the patient level, getting a baseline MRI before leaving the hospital is imperative so that we have a starting point to evaluate and treat them,” explained Fotuhi.
In the just published paper, Dr. Fotuhi and his colleagues warn about neurological issues in patients who suffer from COVID-19, including stroke, seizures, confusion, dizziness, paralysis, and/or coma. Already, two dozen case reports are revealing the impact of COVID-19 on the brains of patients. In fact, one study from Wuhan, China, showed that 45% of patients with severe COVID-19 illness experience marked neurological deficits. Another study from France showed 84% of ICU patients with COVID-19 have positive abnormalities on their neurological examination, and that 15% of patients who leave the ICU have residual “dysexecutive function,” which involves poor attention and difficulty with decision-making and controlling behavior.
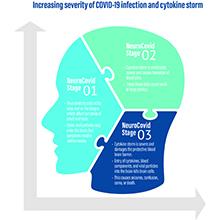
The paper proposes the adoption of a three stage “NeuroCovid” classification scheme to provide a basis from which to build on future hypotheses and investigations regarding SARS-Cov2 and the nervous system. These stages include:
- NeuroCovid Stage I: The virus damage is limited to epithelial cells of nose and mouth and the main symptoms include transient loss of smell and taste.
- NeuroCovid Stage II: The virus triggers a flood of inflammation, called cytokine storm, which begins in the lungs and travels in the blood vessels throughout all body organs. This cytokine storm leads to the formation of blood clots which cause small or large strokes in the brain.
- NeuroCovid Stage III: An explosive level of cytokine storm damages the blood brain barrier, the protective insulation layer in blood vessels of the brain. As a result, blood content, inflammatory markers, and virus particles invade the brain and patients develop seizures, confusion, coma, or encephalopathy.
Fotuhi points out that many patients with COVID-19 may have no noticeable neurological symptoms at first; but in some cases, patients may present with neurological symptoms even before they have fever, cough, or shortness of breath. In addition to having an MRI while at the hospital, he stresses that patients will need to be monitored in a few months after their hospitalization.
“Our experience with previous forms of coronaviruses suggest that in the long-term patients may develop depression, insomnia, Parkinson’s disease, memory loss, or accelerated aging in the brain,” elaborated Fotuhi. “For those recovering from COVID-19, I recommend regular exercise, eating a heart healthy diet, reducing stress, and improving sleep; these are critical ways patients can rejuvenate their brain and minimize having poor outcomes in the future.”
These interventions, along with targeted brain training and neurofeedback therapy, are the main features of Dr. Fotuhi’s 12-week Brain Fitness Program. As published in the Journal of Prevention of Alzheimer’s Disease (2016), 84% of elderly with cognitive impairment who complete this brain rehabilitation program gain improvements in their brain function and many of them experience growth in the parts of their brain for learning and memory. These findings were similar for patients who gained recovery from their persistent post-concussion syndrome. The program will now be tailored for patients suffering from post-COVID neurological issues.
A Harvard- and Johns Hopkins-trained neurologist and neuroscientist, Dr. Fotuhi is widely regarded as an authority in the field of memory, Alzheimer’s disease, concussion treatment, ADHD, and increasing brain vitality at any age.
###
NOTES FOR EDITORS
Full open access review: "Neurobiology of COVID-19" by Majida Fotuhi, Ali Mian, Somayeh Meysami, and Cyrus A. Raji (DOI: 10.3233/JAD-200581), published online (June 2020) in the Journal of Alzheimer's Disease, in advance of publication of Vol. 76, Iss. 1. The full study is openly available at: content.iospress.com/articles/journal-of-alzheimers-disease/jad20058.
Contact
Shawn Flaherty, PR, +1 703-554-3609
Dr. Majid Fotuhi, +1 703-462-9296
About the Journal of Alzheimer's Disease
Now in its 23rd year of publication, the Journal of Alzheimer's Disease (JAD) is an international multidisciplinary journal to facilitate progress in understanding the etiology, pathogenesis, epidemiology, genetics, behavior, treatment, and psychology of Alzheimer's disease. The journal publishes research reports, reviews, short communications, book reviews, and letters-to-the-editor. Groundbreaking research that has appeared in the journal includes novel therapeutic targets, mechanisms of disease, and clinical trial outcomes. JAD has a Journal Impact Factor of 3.517 according to Journal Citation Reports (Web of Science Group, 2019) and is published by IOS Press. j-alz.com







